Please choose a body region on the right for you to pin point the problem area of your body.

Shop by Condition

Shop by Brand
by Dr. Sharon Orrange
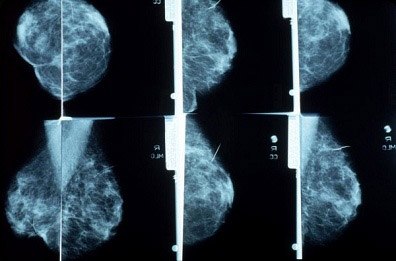
As much as we hear about breast MRI and other new modalities for breast cancer screening it gets confusing for people to sort out what is best for them. To keep it simple, for most of us mammogram is still the best imaging study. Screening mammograms start for most women at age 40 and that's where the debate begins. Every year or every other year mammogram between the age of 40 and 50 depending on your risks, then at the age of 50 we all go to once a year mammogram. Let's start with the most common questions I am asked and get updated on the latest in breast cancer screening.
Which is better Digital or Analog Mammogram? Digital mammography has only been available at most facilities for the last 5 years. For most people the effectiveness is equivalent HOWEVER in pre-menopausal women, women with dense breasts, and women under 55 digital mammography fares better in the diagnosis of breast cancer.
What also matters with mammography? The person reading the mammogram matters! You want a radiologist who spends most of their time doing breast imaging. You can ask who is reading your mammogram and what percentage of their time they spend reading screening mammograms.
Who should get more than just once a year mammogram? ENHANCED SCREENING is recommended by the American Cancer Society for women at high risk for breast cancer. Women at high risk for breast cancer are:
How do I find out if I am considered high risk? You can assess your risk using a well known risk assessment tool. It is published on The National Institutes of Health website (http://www.cancer.gov/bcrisktool/Default.aspx) and this will give you your risk for the next five years. Always discuss your results with your healthcare provider as well.
Who should be tested for BRCA 1 and BRCA 2? These are the inherited mutations in the genes that are involved in hereditary forms of breast and ovarian cancer. The
US Preventive Services Task Force recommends screening for BRCA 1 and 2:
Is it better to get an ultrasound and a mammogram together? This question was asked and answered in a study published in 2008 which looked at screening ultrasound + mammography vs. mammography alone for certain women at risk for breast cancer.
How was high risk defined in this study? BRCA 1 or 2 (+), history of chest, mediastinal or axillary radiation,25% lifetime risk of breast cancer or 5 year risk > 2.5% or > 1.7% and extremely dense breasts. Women with a personal history of breast cancer, atypical ductal or lobular hyperplasia, DCIS, or lobular carcinoma in situ were also included.
What did they find? The good news was that adding a SINGLE screening ultrasound will detect 1.1-7.2 additional cancers per 1000 women with increased breast density. The bad news was this study used physician-performed ultrasound so it s not clear if the results would be the same with non-physician technicians. The other bad news was that the number of false positives increases with ultrasound which results in unnecessary biopsies.
Conclusions about Breast ultrasound + Mammography for screening in high risk women: When physician performed, breast ultrasound increases sensitivity but decreases specificity of cancer screening in high risk women with dense breasts. No guidelines currently recommend screening breast ultrasound.
What about Breast MRI? For those who need "enhanced screening" (criteria listed above) annual screening MRI as adjunct to mammography and clinical breast examination is recommended. Again, there is insufficient evidence for or against the addition of screening ultrasound.
To summarize about Breast MRI (since I am asked about it quite a bit) Current guidelines recommend MRI with mammography in some high risk women. There are no studies of the effect of screening breast MRI on breast cancer mortality that have been published as of yet. Routine breast MRI in everyone is NOT recommended because of the high false positive rates and unnecessary biopsies, in addition to being very expensive. Again, breast MRI is recommended in combination with mammography in women at very high risk of breast cancer.
What about for women with saline or silicone implants? There is still no evidence to suggest that any screening test is better than digital mammogram for those with implants. For questions of whether an implant has ruptured MRI is helpful.
Get $10 off your next order when you sign up to receive our email newsletter.*
Simply enter your email address below!
*Minimum order value of $100. Valid email address to qualify.