
Diabetes is a very serious, lifelong disease. It can create a need for significant lifestyle changes, and if overlooked or left untreated, it can easily cause complications or even death. One of the scariest things about diabetes, however, is that sometimes symptoms don’t appear until well into the course of the disease. Keep a careful eye on your health with regular checkups, and don’t ignore any warning signs, whether it’s symptoms you can’t explain, or blood pressure/blood sugar levels.
 Maybe you’ve heard a lot about how deadly diabetes is, but you don’t understand it. Put simply, diabetes is the resulting condition of the body’s inability to regulate blood sugar. Depending on the cause for this difficulty, one may typically be diagnosed with either Diabetes type 1 or type 2.
Maybe you’ve heard a lot about how deadly diabetes is, but you don’t understand it. Put simply, diabetes is the resulting condition of the body’s inability to regulate blood sugar. Depending on the cause for this difficulty, one may typically be diagnosed with either Diabetes type 1 or type 2.
After eating it’s natural for blood glucose levels to rise briefly; diabetes, or more accurately hyperglycemia, is the term used to describe a blood glucose level that remains high even long after eating. Ordinarily, after eating, organs in the body (the pancreas, primarily) release insulin to move glucose from the blood into the cells. In the case of diabetics, there is a problem with insulin production or effectiveness that makes it difficult to properly transfer glucose out of the blood.
A fasting glucose level, which describes the blood glucose level after eight hours or no food consumption, must be below 126mg/dl; levels higher than 126 mg/dl indicate diabetes. Likewise, a blood glucose level of 200mg/dl or higher two hours after a meal also indicates diabetes.
Essentially, diabetes is the result of blood glucose (sugar) remaining in the bloodstream, instead of being absorbed by the body. Typically, insulin helps with this process; however, a lack of insulin or even an inadequate amount of it will not be able to absorb enough glucose. Additionally, insulin can also lose the ability to help glucose be absorbed, no matter how much insulin is actually present.
While type 2 diabetes is easily the most common, followed distantly by type 1, there is a third type of diabetes known as ‘Gestational Diabetes’. Gestational diabetes only affects pregnant women, typically in the third trimester of their pregnancy, due to increased blood sugar levels. While not a serious condition on its own, gestational diabetes can trigger type 2 diabetes in the future. This is because of the role that body fat and inactivity play in the development of diabetes.
Regardless of the cause of diabetes, the end result is the same: hyperglycemia, or more simply, high blood sugar. Hyperglycemia can cause a number of complications, so consider seeking medical counsel if you develop one or more of the following symptoms:
While fatigue can come from a number of illnesses, it is an important potential indicator of diabetes. Fatigue appears as a symptom of hyperglycemia because of the way the body produces energy; the body depends on glucose to provide energy for the cells, particularly muscle cells. Therefore, in persons with high blood sugar, all of the energy that should be making it into the cells for use simply isn’t, which means the body is not getting an adequate fuel supply. This creates a feeling of fatigue or lethargy.
 Typically when it comes to health and fitness, weight loss is hailed as a good thing. However, the relationship between weight and health is more complicated than that. In the case of diabetics, weight loss can actually be a bad thing. Weight lost from a regular physical exercise regimen is mostly fat, and sometimes is eclipsed by muscle gains, as muscle is heavier than fat. Diabetic bodies, however, which cannot make use of glucose for energy, instead tend to burn muscle mass in addition to fat reserves.
Typically when it comes to health and fitness, weight loss is hailed as a good thing. However, the relationship between weight and health is more complicated than that. In the case of diabetics, weight loss can actually be a bad thing. Weight lost from a regular physical exercise regimen is mostly fat, and sometimes is eclipsed by muscle gains, as muscle is heavier than fat. Diabetic bodies, however, which cannot make use of glucose for energy, instead tend to burn muscle mass in addition to fat reserves.
The body’s digestive system works by absorbing and using whatever nutrients it can, and then flushing the rest; this includes excesses of perfectly good and useful nutrients and is essentially what the daily recommended allowance is. Too much of anything can damage the body; it’s the responsibility of the kidneys to remove excess substances from the body. In the case of hyperglycemia, there is an excess of glucose in the blood, and the kidneys flush as much of it as possible, which translates to a greater and more frequent need to urinate.
A greater need to urinate typically results in a greater need to drink more fluids. Keep in mind that it is the glucose in the blood that needs to be flushed; the water used in urine to flush it is more valuable, and therefore must be more frequently replaced.
 Slow Healing of Wounds
Slow Healing of WoundsEndothelial progenitor cells (EPC) are responsible for repairing injuries via the formation of blood vessels at sites of damage. Diabetic complications can drastically hinder the ability of these cells to perform their duties.
Thrush is a fungal infection. Typically, it occurs in the mouths of infants, but in the case of diabetics, thrush often affects the genital region. Essentially, it is a yeast infection encouraged by excess glucose in the urine. Symptoms of thrush include swelling, redness, and itching, and may be accompanied by thick, whitish discharge.
Elevated levels of blood glucose trigger an absorption of water by the lenses in the eyes. This absorption causes them to swell, which alters their shape and consequently, the ability to focus. While these effects can be reversed with diabetic medication, there are changes that can do permanent damage. For example, extended hyperglycemia weakens the blood vessels of the retina, which can deform them. Once damaged, they release exudate, a protein that can cause permanent damage to the retina, and therefore, vision.
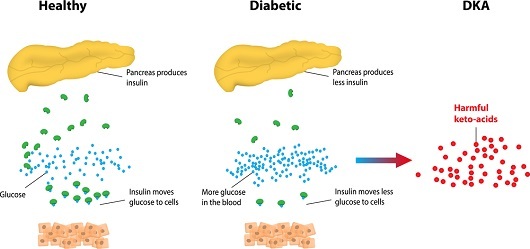 Diabetic ketoacidosis ( DKA ) is among the most severe complications of diabetes. Typically, it arises from type 1 diabetes. As mentioned in the point with the weight loss, when the body cannot turn glucose into the energy the body needs, the body compensates by breaking down fatty acids and proteins in order to generate energy. While this is effective in the short term, it produces acidic ketone bodies, which will eventually turn the blood acidic if their levels increase too much.
Diabetic ketoacidosis ( DKA ) is among the most severe complications of diabetes. Typically, it arises from type 1 diabetes. As mentioned in the point with the weight loss, when the body cannot turn glucose into the energy the body needs, the body compensates by breaking down fatty acids and proteins in order to generate energy. While this is effective in the short term, it produces acidic ketone bodies, which will eventually turn the blood acidic if their levels increase too much.
Fortunately, diabetic ketoacidosis does generate other symptoms. Acidic blood is essentially a hostile environment. It causes damage to a lot of cell tissue. It disrupts the systems of your body in numerous ways. One of the trademark symptoms is acetone breath; it’s more commonly known as ‘fruity-smelling breath’ based on the odor of the chemical acetone, which propagates in an acidic environment. Other symptoms include a loss of appetite, nausea or vomiting, stomach pains, a high body temperature, muscle stiffness and cramps, and a decline in alertness. Sudden and persistent presence of these symptoms should be taken as an immediate warning to seek medical assistance.
Unfortunately, there isn’t a cure for diabetes yet. However, it can be managed by medication and diet and lifestyle changes. For the majority of diabetics (type 2), diabetes can be managed by consuming less glucose and fat in the diet, while engaging in regular exercise. Diabetic medication can also play a large part. In the case of type 1 diabetes, regular insulin injections can keep blood sugar under control; however, low blood sugar, or hypoglycemia, can also cause severe problems, particularly convulsions and even fainting.
In addition to lifestyle changes, there are other risk factors that make one predisposed to diabetes; visceral fat can impede insulin’s ability to function, so regular exercise serves as a preventative measure. Likewise, eating foods low in sugar reduces the amount of glucose that ends up in the bloodstream in the first place. Other factors that can increase the risk of diabetes are genetics (family history) and high blood pressure. While we can’t change the genes we are born with, we can do our best to live healthier, fuller lives. Dietary changes that cut out salt and increase potassium and magnesium, along with other healthy nutrients, can counter high blood pressure. In addition, make sure you monitor your blood sugar and blood pressure daily and schedule regular check-ups with your doctor. Diabetes can definitely change your life, but it doesn’t have to ruin it.
Written by Dianne G.
| Stay Connected! | |
|
Related Articles